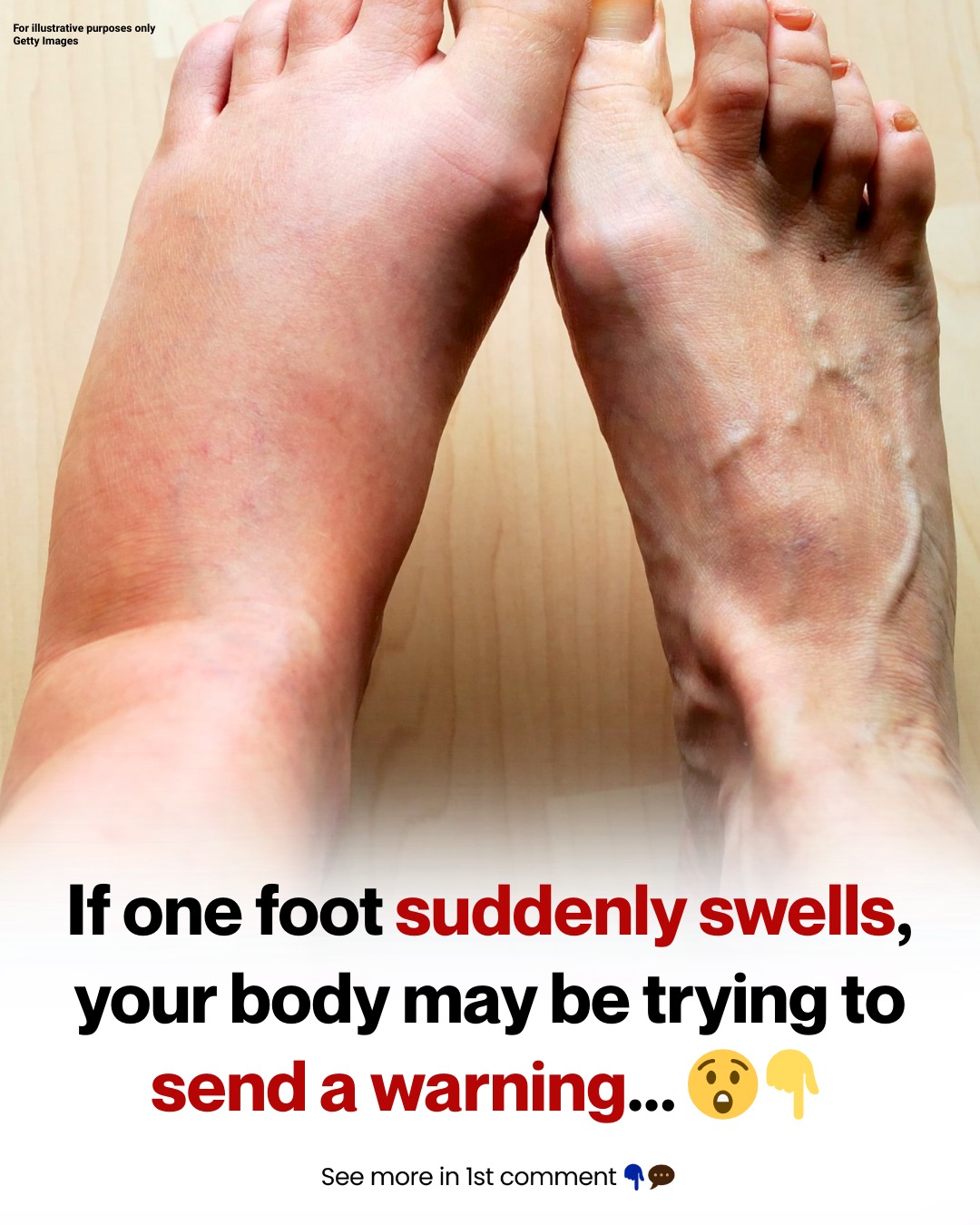
Why swelling happens in the first place
Swelling is usually your body reacting to one of these patterns:
Extra fluid pooling in tissues (common with salt, heat, hormones, or certain conditions)
Inflammation (your immune system responding to injury, irritation, or joint disease)
Circulation problems (blood or lymph fluid not moving back up efficiently)
A blockage or infection (less common but more urgent)
The key clue is often whether it’s one foot or both, and how quickly it appeared.
For illustrative purposes only
The most common causes of swollen feet (and what they often feel like)
1) Fluid retention (everyday edema)
This is one of the most common reasons people notice swelling. The body holds on to water and salt, and gravity pulls fluid down into the ankles and feet.
Common triggers:
Hot weather
High-sodium meals (instant noodles, processed snacks, salty sauces)
Sitting or standing for long periods
Not moving much during travel days
Often feels like: puffiness, tight skin, mild discomfort, usually worse by evening.
2) Poor circulation or vein issues
When veins struggle to push blood back upward, fluid can leak into nearby tissue and cause swelling. This can be more noticeable in people with varicose veins or those who stand a lot.
Often feels like: heaviness, swelling that worsens as the day goes on, sometimes aching.
3) Injury (even if it seems “minor”)
A sprain, strain, bruise, or fracture can cause swelling as part of healing—even if the pain isn’t dramatic at first.
Often feels like: swelling around a specific spot, tenderness, pain when walking, sometimes bruising.
For illustrative purposes only
4) Joint problems (arthritis or gout)
Inflammatory joint issues can cause swelling—often more localized around a toe joint, ankle joint, or the top of the foot.
Often feels like: stiffness, warmth, pain, and swelling focused around a joint.
5) Medication side effects (very common and overlooked)
Some medicines can lead to swelling as a side effect. Examples can include certain blood pressure medications, anti-inflammatory medicines, and others. If swelling started after a new medication, it’s worth discussing with a clinician.
(Do not stop prescribed medication on your own—ask first.)
6) Heart, kidney, or liver conditions (more likely when swelling is persistent)
When the heart isn’t pumping efficiently, or the kidneys/liver aren’t managing fluid balance well, swelling can appear—often in the feet and legs. Swelling is one of the recognized signs seen in heart failure symptom checklists.
Often feels like: persistent swelling, sometimes both legs, may come with weight gain or breathlessness (more urgent).
One swollen foot vs. both: why “one-sided” swelling matters
Swelling in both feet often points to gravity, salt, inactivity, heat, or overall fluid balance issues.
Swelling in one foot/leg—especially if it is sudden, painful, red, or warm—can sometimes indicate something more urgent and should be checked sooner. The NHS lists one-sided swelling with no clear cause, sudden severe swelling, redness/warmth, or fever as reasons to seek urgent help.
For illustrative purposes only
Red flags that should NOT be ignored
Seek urgent medical attention if swelling comes with:
Sudden swelling in one foot/leg with no obvious reason
Redness, warmth, tenderness, or pain (especially one-sided)
Fever, chills, or feeling unwell
Shortness of breath, chest pain, fainting, or coughing blood (emergency)
One important reason clinicians take one-sided swelling seriously is the possibility of deep vein thrombosis (DVT). DVT can cause swelling, pain/tenderness, warmth, and redness/discoloration, and it needs prompt evaluation.
What you can do at home (for mild cases)
If the swelling is mild, you feel well, and there are no red flags:
Elevate
Prop your leg up so your foot is above heart level for 15–20 minutes, 2–3 times a day.
Cold compress
Apply a cool compress for 10–15 minutes if it feels sore or inflamed.
Move the ankle
Try “ankle pumps” (flex foot up/down) and gentle walking to support circulation.
Reduce salt for 24–48 hours
Cut back on salty foods and processed snacks—this can make a noticeable difference.
Hydrate
It sounds backwards, but drinking enough water can help your body regulate fluid better.
Check your shoes
Avoid tight shoes that compress the foot. If footwear suddenly feels tight on one side, that itself is a clue.
Simple prevention habits that actually work
Take a 2–3 minute movement break every hour if you sit or stand a lot
Walk daily (even 20–30 minutes helps circulation)
Keep an eye on sodium (especially if swelling is frequent)
If you travel often, stand/stretch regularly and do ankle circles
For illustrative purposes only
When to see a doctor (even if it doesn’t feel “serious”)
Make an appointment if:
swelling lasts more than a few days
it keeps coming back
you notice skin changes (shiny, stretched, pitting when pressed)
it’s clearly worse on one side without a clear injury
A clinician may ask about timing, recent travel, medications, injury history, and may examine circulation, joints, and skin. Sometimes they’ll recommend tests to rule out infection, clots, or organ-related fluid issues.
A body signal worth listening to
Feet don’t complain loudly—so when they do, it’s often for a reason. Swelling can be harmless, but when it’s persistent, one-sided, sudden, or paired with pain/redness/warmth, it deserves attention rather than normalization.