Millions of women around the world endure debilitating pelvic pain, heavy periods, and unexplained fatigue month after month, often dismissing it as “normal” menstrual discomfort. This silent struggle frequently leads to years of unnecessary suffering, missed work, strained relationships, and emotional exhaustion. The harsh reality is that many delay seeking help due to stigma or lack of awareness, allowing the condition to progress unchecked. But here’s the empowering truth: gaining knowledge about endometriosis can dramatically change your health journey — and there’s a surprising fact about modern management that could make a real difference in your daily life, revealed later in this article.
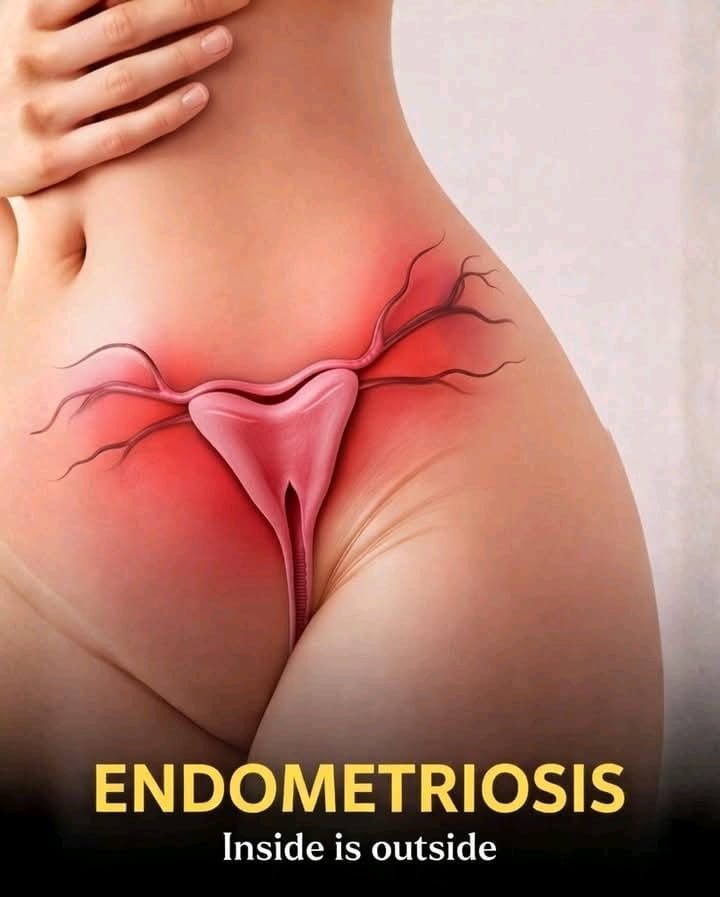
What Is Endometriosis?
Endometriosis is a chronic condition where tissue similar to the lining of the uterus (endometrium) grows outside the uterus. This misplaced tissue commonly appears on the ovaries, fallopian tubes, pelvic lining, and occasionally in other areas.
Like normal endometrial tissue, it thickens, breaks down, and bleeds with each menstrual cycle. However, this blood has no exit route, leading to inflammation, irritation, scar tissue (adhesions), and cysts on the ovaries (endometriomas)
Research shows endometriosis affects approximately 10% of reproductive-age women worldwide — that’s about 190 million individuals globally, according to the World Health Organization.
But that’s not all — the impact goes far beyond physical symptoms.
Common Symptoms of Endometriosis
Pain stands out as the hallmark symptom, yet it varies greatly between women. Many describe it as far more intense than typical period cramps
Here are the most frequently reported signs
Severe menstrual cramps that often begin days before your period and linger afterward
Chronic pelvic or lower back pain that persists throughout the month
Pain during or after sexual intercourse (dyspareunia)
Heavy menstrual bleeding or spotting between periods
Difficulty conceiving or infertility challenges
Digestive problems like bloating, constipation, or diarrhea — especially during menstruation
Fatigue, low energy, and sometimes nausea around periods
Here’s the frustrating part: These symptoms often overlap with other conditions like IBS or pelvic inflammatory disease. Studies indicate that diagnosis can take 7–10 years on average, leaving many women in prolonged distress.
What Causes Endometriosis?
The exact cause remains under investigation, but experts point to several contributing factors.
Key theories include:
Retrograde menstruation — Menstrual blood flows backward through the fallopian tubes into the pelvic cavity instead of exiting the body (a process common in most women, but only some develop endometriosis).
Genetic predisposition — If your mother or sister has endometriosis, your risk increases significantly.
Immune system issues — The body may not effectively clear misplaced endometrial tissue.
Hormonal factors — Estrogen promotes the growth of this tissue.
Importantly, endometriosis is not caused by lifestyle choices, and it’s not preventable through personal actions alone. It’s a complex condition influenced by multiple biological factors.How Is Endometriosis Diagnosed?
Diagnosis often proves challenging due to symptom overlap with other disorders.
Healthcare providers typically start with
A thorough medical history, including family background and symptom patterns
Pelvic examination to check for abnormalities
Imaging like transvaginal ultrasound or MRI to visualize potential lesions
In many cases, laparoscopy — a minimally invasive surgery — provides definitive confirmation by allowing direct visualization and tissue sampling.
Recent advances in imaging have improved non-invasive options, helping reduce delays in some settings.
Endometriosis and Fertility: What You Need to Know
Endometriosis ranks among the top causes of infertility.
Research indicates that 30–50% of women with endometriosis face conception difficulties. Inflammation, scar tissue, and adhesions can block fallopian tubes, disrupt egg release, or hinder implantation.
The encouraging news? Many women with endometriosis conceive naturally or with assistance like fertility treatments. Early intervention often improves outcomes.
Management and Treatment Options
While no cure exists, effective strategies can significantly control symptoms and enhance quality of life.
Common approaches include
Pain relief — Over-the-counter NSAIDs (like ibuprofen) for mild cases; prescription options for more severe pain.
Hormonal therapies — Birth control pills, progestins, or hormonal IUDs to suppress menstruation and reduce tissue growth.
Surgery — Laparoscopic removal of lesions for severe cases or when fertility is a priority.
Lifestyle support — Regular exercise, stress reduction techniques, and good sleep hygiene.
Treatment plans are highly personalized — always consult a healthcare professional to find what works best for you.
Here’s the interesting part: Emerging evidence suggests diet may play a supportive role in managing symptoms.
←PreviousNext→The Role of Diet in Managing Endometriosis Symptoms
While diet alone cannot treat endometriosis, research highlights potential benefits from certain patterns.
Anti-inflammatory foods — Fruits, vegetables, whole grains, and omega-3-rich foods (like fish, nuts, seeds) may help reduce inflammation.
Limiting certain items — High intake of red meat, processed foods, and excessive caffeine or alcohol might worsen symptoms in some women.
Fiber-rich choices — High-fiber diets support hormone balance and gut health.
Evidence from recent reviews points to benefits from Mediterranean-style eating or low-FODMAP approaches for gastrointestinal symptoms. Always discuss dietary changes with a doctor or registered dietitian
Here are some practical, actionable tips you can try today:
Track your symptoms and diet for 4–6 weeks to identify personal triggers.
Incorporate more colorful vegetables and fruits daily.
Stay hydrated and aim for balanced, regular meals.
Consider gentle exercise like walking or yoga to ease pain and stress.
Join online support communities for shared experiences and tips.
Living with Endometriosis: You’re Not Alone
This chronic condition can affect work, relationships, and mental health — but many women thrive with proper support.
Building a care team, connecting with support groups, and practicing self-compassion make a huge difference. Raising awareness reduces stigma and empowers earlier action.
Frequently Asked Questions (FAQ)
Q: Can endometriosis go away on its own?
A: No, it’s a chronic condition. Symptoms may fluctuate, but without management, they often persist or worsen.
Q: Does endometriosis always cause infertility?
A: Not always — many women with endometriosis conceive without issues, though it raises the risk. Fertility treatments can help.
Q: Is endometriosis linked to ovarian cancer?
A: Endometriosis slightly increases the risk of certain ovarian cancers, but the overall risk remains low. Regular check-ups are recommended.
Disclaimer: This article is for informational purposes only and does not replace professional medical advice. Always consult a qualified healthcare provider for diagnosis, treatment, or personalized guidance regarding endometriosis or any health concern. Individual experiences vary, and evidence-based care is essential.